Abstract
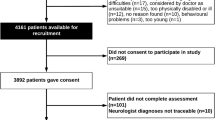
Many patients with a diagnosis of neurological disease, such as multiple sclerosis, have symptoms or disability that is considered to be in excess of what would be expected from that disease. We aimed to describe the overall and relative frequency of symptoms ‘unexplained by organic disease’ in patients attending general neurology clinics with a range of neurological disease diagnoses. Newly referred outpatients attending neurology clinics in all the NHS neurological centres in Scotland, UK were recruited over a period of 15 months. The assessing neurologists recorded their initial neurological diagnoses and also the degree to which they considered the patient’s symptoms to be explained by organic disease. Patients completed self report scales for both physical and psychological symptoms. The frequency of symptoms unexplained by organic disease was determined for each category of neurological disease diagnoses. 3,781 patients participated (91% of those eligible). 2,467 patients had a diagnosis of a neurological disease (excluding headache disorders). 293 patients (12%) of these patients were rated as having symptoms only “somewhat” or “not at all” explained by that disease. These patients self-reported more physical and more psychological symptoms than those with more explained symptoms. No category of neurological disease was more likely than the others to be associated with such symptoms although patients with epilepsy had fewer. A substantial proportion of new outpatients with diagnoses of neurological disease also have symptoms regarded by the assessing neurologist as being unexplained by that disease; no single neurological disease category was more likely than others to be associated with this phenomenon.

Similar content being viewed by others
References
Aring C (1965) Observations on multiple sclerosis and conversion hysteria. Brain 88:663–674
Association of British Neurologists (Service Committee) (1991) UK audit of the care of common neurological disorders. Association of British Neurologists, London
Benbadis S, Agrawal V, Tatum WO (2001) How many patients with psychogenic nonepileptic seizures also have epilepsy? Neurology 57:915–917
Caplan LR, Nadelson T (1980) Multiple sclerosis and hysteria. Lessons learned from their association. JAMA 243:2418–2421
Carson AJ, Ringbauer B, Stone J, McKenzie L, Warlow C, Sharpe M (2000) Do medically unexplained symptoms matter? A prospective cohort study of 300 new referrals to neurology outpatient clinics. J Neurol Neurosurg Psychiatry 68:207–210
Carter AB (1967) The functional overlay. Lancet 2:1196–1200
Crimlisk HL, Bhatia K, Cope H, David A, Marsden CD, Ron MA (1998) Slater revisited: 6 year follow up study of patients with medically unexplained motor symptoms. BMJ 316:582–586
Eames P (1992) Hysteria following brain injury. J Neurol Neurosurg Psychiatry 55:1046–1053
Hopkins A, Menken M, DeFriese G (1989) A record of patient encounters in neurological practice in the United Kingdom. J Neurol Neurosurg Psychiatry 52:436–438
Lecompte D (1987) Organic disease and associated psychopathology in a patient group with conversion symptoms. Acta Psychiatr Belg 87:662–669
Lempert T, Dieterich M, Huppert D, Brandt T (1990) Psychogenic disorders in neurology: frequency and clinical spectrum. Acta Neurol Scand 82:335–340
Maddison P (2005) Neurology training in the United Kingdom: a diagnostic analysis of over 5,000 patients. J Neurol 252:605–607
Merskey H, Buhrich NA (1975) Hysteria and organic brain disease. Br J Med Psychol 48:359–366
Onofrj M, Bonanni L, Manzoli L, Thomas A (2010) Cohort study on somatoform disorders in Parkinson disease and dementia with Lewy bodies. Neurology 74:1598–1606
Perkin GD (1989) An analysis of 7,836 successive new outpatient referrals. J Neurol Neurosurg Psychiatry 52:447–448
Sharpe M, Mayou R, Walker J (2006) Bodily symptoms: new approaches to classification. J Psychosom Res 60:353–356
Sharpe M, Stone J, Hibberd C, Warlow C, Duncan R, Coleman R, Roberts R, Cull R, Pelosi A, Cavanagh J, Matthews K, Goldbeck R, Smyth R, Walker A, Walker J, Macmahon A, Murray G, Carson A (2010) Neurology out-patients with symptoms unexplained by disease: illness beliefs and financial benefits predict 1-year outcome. Psychol Med 40:689–698
Stevens DL (1989) Neurology in Gloucestershire: the clinical workload of an English neurologist. J Neurol Neurosurg Psychiatry 52:439–446
Stone J, Carson A, Duncan R, Coleman R, Roberts R, Warlow C, Hibberd C, Murray G, Cull R, Pelosi A, Cavanagh J, Matthews K, Goldbeck R, Smyth R, Walker J, Macmahon AD, Sharpe M (2009) Symptoms ‘unexplained by organic disease’ in 1,144 new neurology out-patients: how often does the diagnosis change at follow-up? Brain 132:2878–2888
Stone J, Carson A, Duncan R, Roberts R, Warlow C, Hibberd C, Coleman R, Cull R, Murray G, Pelosi A, Cavanagh J, Matthews K, Goldbeck R, Smyth R, Walker J, Sharpe M (2010) Who is referred to neurology clinics? The diagnoses made in 3,781 new patients. Clin Neurol Neurosurg 112:747–751
Wade DT, Halligan PW (2004) Do biomedical models of illness make for good healthcare systems? BMJ 329:1398–1401
Wiles CM, Lindsay M (1996) General practice referrals to a department of neurology. J Royal Coll Phys 5:426–431
Young WB, Gangal KS, Aponte RJ, Kaiser RS (2007) Migraine with unilateral motor symptoms: a case-control study. J Neurol Neurosurg Psychiatry 78:600–604
Acknowledgments
We would like to thank Carina Hibberd and all the neurologists and general practitioners who took part in this study; S Tennant, L Alder, J Sim, M Selkirk, D McConachie—the researchers who administered the questionnaires. This study was funded by the Clinical Research Audit Group (CRAG) NHS Scotland and the Chief Scientist Office, Health Department of the Scottish Government.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Appendix: Guidance given to doctors on ‘What we mean by organic disease’
Appendix: Guidance given to doctors on ‘What we mean by organic disease’
The following is meant as a guide for this study and we are aware that any divisions like this are imperfect. Many patients have a mixture of symptoms, syndromes or disease and the final coding is your decision based on these guidelines.
“Not organic disease” for the purpose of this study: tension headache; aetiologically controversial symptom ‘syndromes’ (e.g., chronic fatigue syndrome, fibromyalgia, irritable bowel syndrome); physiologically explained processes which are thought to be linked to emotional symptoms (e.g., hyperventilation); emotional disorders (e.g., depression, anxiety, panic disorder).
‘Organic disease’ for the purpose of this study: migraine; any neurological disorder with a known pathological basis; Neurological disorders with defined and characteristic features but without a clear pathological basis (e.g., Gilles de la Tourette syndrome, idiopathic focal dystonia); Physiological explained processes NOT linked to emotional symptoms (e.g., micturition syncope); psychotic disorder.
Rights and permissions
About this article
Cite this article
Stone, J., Carson, A., Duncan, R. et al. Which neurological diseases are most likely to be associated with “symptoms unexplained by organic disease”. J Neurol 259, 33–38 (2012). https://doi.org/10.1007/s00415-011-6111-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-011-6111-0