Abstract
To determine self-reported health status in non-dystrophic myotonias (NDM) and its relationship to painful myotonia and fatigue. In a cross-sectional study, 32 NDM patients with chloride and 30 with sodium channelopathies, all off treatment, completed a standardised interview, the fatigue assessment scale (FAS), and the 36-item Short-Form Health Survey (SF-36). Beside formal assessment of pain, assessment of painful or painless myotonia was determined. The domain scores of the SF-36 were compared with Dutch community scores. Apart from the relationship among SF-36 scores and (1) painful myotonia and (2) fatigue, regression analyses in both NDM groups were conducted to determine the strongest determinants of the SF-36 domains general health perception, physical component (PCS) and mental component summary (MCS). All physically oriented SF-36 domains in both NDM groups (P ≤ 0.01) and social functioning in the patients with sodium channelopathies (P = 0.048) were substantially lower relative to the Dutch community scores. The patients with painful myotonia (41.9%) scored substantially (P < 0.05) lower on most SF-36 domains than the patients without painful myotonia (58.1%). Fatigued patients (53.2%) scored substantially lower (P ≤ 0.01) on all SF-36 domains than their non-fatigued counterparts (46.8%). The regression analysis showed that fatigue was the strongest predictor for the general-health perception and painful myotonia for the physical-component summary. None of the patients showed below-norm scores on the domain mental-component summary. The impact of NDM on the physical domains of patients’ health status is substantial, and particularly painful myotonia and fatigue tend to impede their physical functioning.
Similar content being viewed by others
Introduction
Non-dystrophic myotonias (NDM) are caused by mutations in genes encoding the skeletal muscle chloride (CLCN1) or sodium channel (SCN4A). Mutations in CLCN1 are responsible for recessive and dominant myotonia congenita (recessive MC [MIM 160800] and dominant MC [255700]), and mutations in SCN4A for paramyotonia congenita (PC [MIM 168300]) and potassium-aggravated myotonias (PAM [MIM 608390]) [29].
The key symptom of MC is myotonia, and especially patients with recessive MC show a combination with transient paresis [4]. Both symptoms improve with continuing exercise, which is referred to as the warm-up phenomenon [9, 26]. Conversely, in PC myotonia worsens with continuing exercise. Muscle weakness is also observed in PC and is mostly elicited by cold or prolonged exercise [10]. Myotonia in PAM is clinically characterised by unusual features such as temporal fluctuation (myotonia fluctuans), permanent myotonia (myotonia permanens) or acetazolamide-responsive myotonia (acetazolamide-responsive myotonia congenita) [19, 27, 35].
Myotonia in NDM is often described as painless muscle stiffness [12]. However, Becker found 15% of his patients with recessive MC to report pain complaints [4]. Also, a fluctuating form of dominant MC, acetazolamide-responsive myotonia congenita and the V445M sodium channel mutation were all associated with painful myotonia; thus, pain appears to be a recurrent symptom in NDM. [4, 28, 35, 37].
Another symptom in neuromuscular diseases is fatigue. Although initially underreported in neuromuscular disorders, fatigue has now been established in post-polio syndrome, immune-mediated polyneuropathies, myasthenia gravis, facioscapulohumeral muscular dystrophy, myotonic dystrophy, and type-I hereditary motor and sensory neuropathy [5, 15, 20, 24, 32]. Our clinical experience has taught us that also patients with NDM may complain of fatigue.
Despite their symptoms and signs, NDMs are considered to be “benign diseases” with possible influences on the patients’ ability to perform activities of daily living, affecting their social participation [18]. This explains why to date no clinical reports are available that have systematically examined the effects NDM has on the patients’ health status, where health status is defined as the impact of the disease on a patient’s physical, psychological and social functioning [6]. The presence of painful myotonia and fatigue in patients with NDM and their impact on the patients’ health status has likewise not been systematically investigated. Therefore, we investigated the impact of NDM on health status. We additionally examined the presence and effects of painful myotonia and fatigue and, finally, performed regression analyses to investigate the contribution of various determinants assumed to impair the patients’ physical, psychological and social functioning.
Patients and methods
Patients
In March 2005 neurologists across The Netherlands as well as the VSN, the Dutch patient association for neuromuscular diseases, were requested to report all patients with a clinical suspicion of NDM to our research group for a full year. Inclusion criteria were age (≥18 years), a diagnosis of NDM according to established clinical criteria and needle-EMG evidence of myotonic discharges [17]. Exclusion criteria were a clinical or genetic diagnosis of type-1 or type-2 myotonic dystrophy or primary periodic paralysis, serious co-morbidity, unwillingness or inability to reduce or stop drug therapy for myotonia during the study and no detectable mutations in CLCN1 or SCN4A.
The 1-year recruitment period yielded a total of 97 potentially eligible patients. Nine patients were unable to participate due to transportation problems. Based on the selection criteria, another 26 patients were excluded: 7 had a primary periodic paralysis, 12 serious co-morbidity, 5 were unwilling to reduce and stop myotonia-related drug therapy, and 2 did not present clinical signs of myotonia and lacked myotonic discharges (needle-EMG). All remaining 62 patients demonstrated DNA mutations in either CLCN1 (n = 32) or SCN4A (n = 30) [33, 34]. The study was approved by the Medical Ethics Committee of the Radboud University Nijmegen Medical Centre, and all patients gave their written informed consent prior to their participation.
Examination procedures
Standardised interview
With the standardised interview the following characteristics of all NDM patients were established: age, gender, duration of symptoms, frequency, pattern (reduction or augmentation of myotonia after repetitive movements) and severity of the myotonia [Numerical Rating Scale (NRS), range 1–10; 1 means almost no myotonia and 10 means very serious myotonia], changes in severity, presence of muscle weakness, presence of painful or painless myotonia and eventually the severity of the painful myotonia (NRS, range 1–10, 1 means almost no painful myotonia and 10 means very serious painful myotonia).
Painful myotonia
We used the outcome of the standardised interview to dichotomise patients with painless and those with painful myotonia. Patients with painful myotonia were also asked about the severity of their pain (NRS, range 1–10).
Fatigue assessment scale
Fatigue was assessed with the ten-item self-reported fatigue assessment scale (FAS) [21]. Five items probe physical and five mental fatigue. Each item is scored on a 5-point Likert scale with the total score ranging from 10 to 50. Higher scores indicate higher fatigue levels. The scale’s validity and reliability of the FAS were good [7, 8, 21]. We took FAS scores equal to or higher than 22 to be indicative of fatigue and used this as the cutoff score to dichotomise fatigued and non-fatigued NDM patients [8].
Short-Form 36-Item Health Survey
Patients completed the Short-Form 36-Item Health Status Survey (SF-36, Dutch version), a generic questionnaire to establish patients’ self-reported health status [1, 38]. It appraises the following domains: physical functioning (ten items), role functioning physical (4), role functioning emotional (3), social functioning (2), body pain (2), mental health (5), vitality (4), general-health perception (5), and change in health, which is scored separately [38]. The number of response categories per item ranges from two to six. Each domain has a scoring range of 0–100 with higher scores, indicating better health or functioning and less body pain. The scale’s physical component summary (PCS) and mental component summary (MCS) scores were also calculated using the reported means, standard deviations and factor-score coefficients derived from the general Dutch population [1, 38–40]. The PCS captures the individual’s overall physical functioning by considering reported limitations in care, physical, social and role activities, amount of pain, and level of energy. The MCS reflects the respondent’s overall mental functioning by considering the frequency of psychological distress and limitations in usual social and role activities due to emotional problems [39]. A linear T score transformation method was used so that the PCS had a mean of 49.7 (SD 9.3), and the MCS had a mean of 52.1 (SD 9.6), as reported for the general Dutch population [1, 38–40]. The SF-36 has been shown to have a good validity and reliability [1, 38–40]. For our comparative analyses, we used the reported mean (SD) SF-36 domain scores of a random, Dutch nationwide sample of 1,742 healthy individuals consisting of 976 men and 766 women with a mean age of 47.6 years (18.0 years; range 16–94 years) [1, 40].
Statistical analysis
Validity and reliability
Prior to the health status analyses, we tested the validity and reliability of the scales used.
Validity was determined by means of Spearman’s rank correlation tests among (1) the various SF-36 dimensions, (2) the SF-36 dimension vitality and FAS and (3) the SF-36 domain body pain and painful myotonia. The reliability of the SF-36 and FAS was estimated by calculating the internal consistency (Cronbach’s α). A Cronbach’s α ≥ 0.7 is considered as having a good reliability [22].
SF-36 values
The mean SF-36 domain and summary (PCS and MCS) values for (1) chloride and sodium channelopathies, (2) the fatigued and the non-fatigued group and (3) the painful and painless myotonia group were compared with Dutch community scores (Student’s t test for independent groups) [1, 40]. In addition, the SF-36 domain scores of the patients with a chloride channelopathy were compared with those with a sodium channelopathy, the fatigued patients were compared with non-fatigued patients, and those patients with painful myotonia were compared with their painless counterparts (Student’s t test for independent groups) [1, 40].
Regression analysis
In both NDM groups linear regression analyses were performed to determine which variable had the greatest impact on the patients’ general health perception, PCS and MCS (dependent variables). Age, gender, duration of symptoms, frequency of myotonia, its pattern after repetitive contractions, myotonia severity and changes in severity, presence of muscle weakness, presence of painful myotonia, severity of the pain and the FAS were considered as explanatory variables. Prior to the regression analyses, the distribution pattern of the dependent variables were examined and, if necessary, a transformation of the values was carried out to obtain a normal distribution pattern. Univariate regression analyses were conducted to reveal those independent variables that were related to dependent variables, separately. This was achieved through a systematic evaluation of constructed graphs with linear regression studies that included a restricted cubic spline function on the independent variable [14]. Subsequently, separate multivariate linear regression analyses were performed for each dependent variable, using the stepwise method including only the independent variables that had shown P ≤ 0.2 in the univariate analyses. The strength of the association between the dependent variable and the independent variables was presented as R 2: the fraction of variance explained by the independent variables from the regression model. All analyses were performed using Stata 7.0 for Windows 2000 (Stata Corp., College Station, TX). A value of P < 0.05 was considered statistically significant.
Results
Interview outcomes
Table 1 shows the basic characteristics of all NDM patients obtained during the standardised interview. All patients complained of myotonia, and the majority (96.9% in chloride and 83.3% in sodium channelopathies) reported daily complaints. All the patients with chloride channelopathies reported a decrease in myotonia after repetitive contractions, which was 50.0% for the patients with a sodium channelopathy, while the other half indicated an increase (paradoxical myotonia). Although ten patients in the chloride group and eight patients in the sodium group used drugs to relieve myotonia before the study, both groups claimed the severity of their myotonia had increased since the onset of symptoms. Over half of all patients with sodium channelopathies (56.7%) and about 30% (28.1%) of the patients with chloride channelopathies characterised their myotonia as painful (χ2 = 5.18, P = 0.02). Finally, 75% of the chloride channelopathies versus 37% of the sodium channelopathies experienced muscle weakness (χ2 = 9.26, P = 0.002).
Incidence painful myotonia
Twenty-six (41.9%) patients reported painful myotonia with a mean NRS score of 6.1; 36 patients (58.1%) reported painless myotonia. There was no relationship between the presence of painful myotonia and gender (χ2 = 0.287, P = 0.670) or between the presence of painful myotonia and age (r = −0.07, P = 0.60).
Fatigue rates by FAS
Based on their FAS scores, 33 (53.2%) patients were classified as fatigued (FAS 27.2 ± 4.3) and 29 (46.8%) as non-fatigued (FAS 16.2 ± 3.5). The FAS scores showed no relationship with gender (r = 0.10, P = 0.440) or age (r = −0.05, P = 0.70).
FAS and SF-36 validity and reliability scores
The matrix in Table 2 shows correlations among (1) the various SF-36 domains, (2) the SF-36 domain vitality and the FAS and (3) the SF-36 domain body pain and painful myotonia for the two NDM groups separately. For most SF-36 dimensions significant correlations were obtained. In both groups the SF-36 scores for vitality (higher scores mean better vitality) correlated inversely with the FAS scores (higher scores mean more fatigued), and the SF-36 scores for body pain (lower scores mean more pain) correlated inversely with painful myotonia (higher scores mean more pain). Table 2 also shows the internal consistencies for the SF-36. For all SF-36 dimensions, good reliability scores (Cronbach’s alpha ≥ 0.7) were obtained. Cronbach’s alpha for the FAS was also good: 0.81 for chloride and 0.90 for sodium channelopathies.
SF-36 outcomes
Chloride and sodium channelopathies
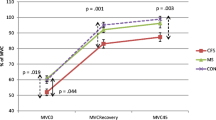
Compared with the Dutch community scores, the means for the physically oriented SF-36 domains (physical functioning, role functioning physical, vitality and general health perception) and the corresponding PCS means were notably lower (P ≤ 0.01) in both NDM groups, indicative of an inferior health status in the patients (Fig. 1a). The means for the more mentally oriented SF-36 domains (role functioning emotional, social functioning, mental health and body pain) and MCS were comparable with Dutch community scores, with social functioning in the patients with sodium channelopathies (P = 0.048) as the only exception. The body pain scores in the chloride group were even significantly higher (indicating less pain) than in the Dutch community (P = 0.014). The SF-36 domain scores and the component scores did not differ between the two NDM groups, with the exception of the body pain scores, which were significantly lower (indicating more pain) in the sodium channelopathy group (P = 0.032).
a comparison of the mean values of the 36-item Short-Form health survey profiles (SF-36) of the patients with NDM (n = 62) per subtype and the mean values for the Dutch community. b The effect of painful myotonia on the patients’ mean scores on the SF-36 versus the reported means for the Dutch community. c The effect of fatigue on the patients’ mean scores of the SF-36 scores versus the reported mean for the Dutch community. NDM non-dystrophic myotonia. PhF physical functioning; RFPh role functioning physical, RFE role functioning emotional, SF social functioning, BP body pain, MH mental health, Vit vitality, GHP general health perception, PCS physical component summary, MCS mental component summary. *P < 0.05
Painful and painless myotonia
Painful myotonia was associated with a significant decrease (P ≤ 0.0001) of all SF-36 domain scores relative to the Dutch community scores, except for the domains role functioning emotional, mental health and MCS (Fig. 1b). The values for role functioning emotional, social functioning, body pain and mental health for the patients that did not report painful myotonia were equal to or higher than the Dutch community scores, whereas their means for physical functioning, general health perception and PCS were significantly (P ≤ 0.048) lower. The pain group showed significantly lower (P ≤ 0.034) mean scores than the non-pain group for role functioning physical, social functioning, body pain, vitality, general health perception and PCS.
Fatigued and non-fatigued patients
All SF-36 domain scores of the fatigued patients were significantly lower (P ≤ 0.01) than the Dutch community scores, except for the domains role functioning emotional, mental health and body pain (Fig. 1c). The means for the non-fatigued patients were equal or higher than the Dutch community scores, apart from the mean for physical functioning (P = 0.02). All SF-36 domain and summary scores of the fatigued patients were substantially lower (P ≤ 0.01) than those found than their non-fatigued counterparts (Fig. 1c).
Regression analysis
As the MCS scores (reflecting overall mental functioning) for our NDM patients closely resembled the Dutch community scores, we restricted our regression analyses to general health perception and PCS (see Fig. 1a). The results of the analyses are shown in Fig. 2. In the chloride group, 45% of the general health perception scores and 45% of the PCS scores were explained by the explanatory variables. The variance proportions obtained in the sodium group were higher: 77% for general health perception and 71% for PCS. Fatigue proved the strongest predictor of general health perception (P ≤ 0.01 for chloride and P ≤ 0.0001 for sodium channelopathies). In the sodium group the pattern of myotonia (P = 0.001), gender (P = 0.002), painful myotonia (P = 0.009) and duration of symptoms (P = 0.019) also significantly contributed to the model. Painful myotonia was the strongest contributor to the PCS score in the chloride channelopathies (P = 0.001), in whom fatigue was also a significant (P = 0.045) contributor. In sodium channelopathies, painful myotonia (P = 0.018), fatigue (P = 0.018) and pattern of myotonia (P = 0.023) were also significant contributors to the PCS score.
Discussion
Despite the general notion that NDMs are benign diseases, the current cross-sectional study demonstrates that the symptoms of these patients do greatly impact their self-reported health status. To our knowledge, ours is the first study to investigate health status in a large group of genetically confirmed NDM patients. The scores of the NDM patients on the scale’s physically oriented domains were substantially lower than the scores reported for the Dutch community (Fig. 1a), reflecting a poorer clinical condition for the patients [1, 38–40]. In addition, 42% of the patients characterised their myotonia as painful and, based on their FAS scores, 53% could be classified as being fatigued. Furthermore, both painful myotonia and fatigue were associated with a significant decrease in almost all SF-36 domain scores (Fig. 1b and c). Finally, our regression analyses revealed that in our sample fatigue was the strongest predictor of low general health perceptions, while painful myotonia best predicted low overall physical functioning (Fig. 2).
The relatively low scores we found in our NDM patients for the physical domains of the SF-36 closely resemble the scores of other chronic diseases like type-II diabetes mellitus, myocardial infarction and angina pectoris with hypertension, as reported in the USA population by the constructors of the SF-36 [39]. In contrast, most of the NDM patients’ scores on the scale’s mental domains and its mental component score were quite similar to the Dutch community scores [1, 38–40]. Studies of elderly patients with chronic conditions, including various peripheral neuropathies and eight chronic medical disorders, also found lower scores on the SF-36 physical dimensions and an unaltered mental state [16, 20, 30]. Presumably, these patients are more preoccupied by changes in their physical status, making them more focused on physical disabling symptoms. Since NDM is a chronic and presumably indolent, progressive disease, it is possible that patients might learn to cope with their limitations. Indirect support for this hypothesis is found in studies of more pronounced progressive chronic illness, such as myotonic dystrophy, ALS, Parkinson's disease and multiple sclerosis. Here, the SF-36 showed the patients’ emotional and mental states to be more affected, although involvement of the central nervous system could not be excluded [3, 23, 25, 31, 36].
The physical domains of the SF-36 of the NDM patients with painful myotonia were substantially more affected than those of the patients with painless myotonia. Pain had earlier been observed to correlate with the physical domains of the SF-36 in other slowly progressive neuromuscular diseases [2]. Fatigue resulted even in a substantial decrease of all SF-36 domains. A negative impact of fatigue on health status was reported earlier in some chronic neurological diseases and various muscular dystrophies [11, 13, 15]. On the other hand, NDM patients without pain or fatigue often had similar or even higher SF-36 scores (better health condition) than the normal Dutch population. This confirms earlier assumptions that there indeed is a group of NDM patients with only a minor or no impact on their health status.
Since Aaronson et al. [1] studied the SF-36 domain scores in different age classes of the Dutch population and detected lower scores with increasing age, age differences among the Dutch population, the NDM population and the NDM subgroups should be discussed in the evaluation of the results. However, since our data showed no correlation between age and the domains of the SF-36 (data not shown), including the physical-component summary and the general-health perception, age differences do not appear to play a role. Furthermore, the mean age of the total NDM population (42.3 ± 11.9 years) is not significantly higher than the mean age of the Dutch population studied by Aaronson (47.6 ± 18.0 years) [1]. Therefore, the lower SF-36 scores of our NDM population could not be caused by age differences. Also, the mean age of the two NDM subgroups (painful myotonia versus painless myotonia and fatigued versus non-fatigued) showed no significant differences. Only the NDM subgroup chloride versus sodium channelopathies showed a significant difference in age: chloride channelopathies were significantly older (Table 1). This is the only group in which we could not pertinently rule out an influence of age differences.
As explained in the introduction, NDMs are not a single disease. However, in this manuscript we only compared chloride with sodium channelopathies. Of course, for more thorough genotype-phenotype correlation studies, a further subdivision should be made. Since the goal of this manuscript was not to describe the different diseases as such but the burden of the total NDM group in daily life and the fact that we have only seen small groups for the different diseases, which makes the groups possibly too small for statistical analysis, we did not analyse more detailed genotype-phenotype correlations.
Some permanent muscle weakness may be a feature of NDM, especially in recessive myotonia congenita and some sodium channelopathies. This could be a confounder. However, since most patients with recessive myotonia congenita experience transient paresis, chronic muscle weakness is very difficult to measure in this group. In the sodium channelopathies all patients showed a maximum MRC sum score (data not presented). Furthermore, none of the patients showed such severe myotonia that muscles became functionally weak. We therefore only used standardised interview parameters in the regression analyses. We used different variables, including frequency of myotonia, severity of myotonia, and muscle weakness, as explanatory variables. None of these, in contrast to fatigue and pain, were a significant variable for the variance of the general health perception or the physical component summary.
Prior to this study, no valid and reliable health status measures had been obtained in patients with NDM. We opted for the SF-36 because of its brevity, its extensive use in clinical studies and its good psychometric properties [1, 38–40]. We selected the FAS to measure fatigue because of its one-dimensionality, ease of use and proven validity and reliability [7, 8, 21]. The scales’ good content validity and reliability make them potentially useful endpoints for future randomised clinical trials that evaluate the efficacy of and responsiveness to drug treatments such as mexiletine.
Despite the solidity of our nationwide findings, it needs to be noted that we did not evaluate the test-retest reliability for the SF-36 and FAS, a psychometric omission future research projects in this field should correct. Furthermore, five patients were unwilling to reduce and stop their drug therapy, and nine patients had transportation problems, including one patient who was severely handicapped. This means that there is a potential bias in this study. Possibly some patients with more severe myotonia have not been assessed. However, these patients may even have a worse health status than the rest.
In summary, the current study shows that NDM substantially affects the patients’ physical health status, with painful myotonia and fatigue being the strongest predictors of the deficits. Beside direct measurements of myotonia, it is recommended that future intervention studies in patients with NDM should also use the SF-36 and FAS to establish the efficacy of the therapeutic regimes under study.
References
Aaronson NK, Muller M, Cohen PD et al (1998) Translation, validation, and norming of the Dutch language version of the SF-36 Health Survey in community and chronic disease populations. J Clin Epidemiol 51:1055–1068
Abresch RT, Carter GT, Jensen MP, Kilmer DD (2002) Assessment of pain and health-related quality of life in slowly progressive neuromuscular disease. Am J Hosp Palliat Care 19:39–48
Antonini G, Soscia F, Giubilei F et al (2006) Health-related quality of life in myotonic dystrophy type 1 and its relationship with cognitive and emotional functioning. J Rehabil Med 38:181–185
Becker PE, Knussmann R, Kuhn E (1997) Myotonia congenita and syndromes associated with myotonia: clinical-genetic studies of the nondystrophic myotonias. In: Becker PE, Lenz W, Vogel F, Wendt GG (eds) Topic in human genetics, vol 3. Thieme, Stuttgart
Berlly MH, Strauser WW, Hall KM (1991) Fatigue in postpolio syndrome. Arch Phys Med Rehabil 72:115–118
De Vries J (2001) Quality of life assessment. In: Vingerhoets AJJM (ed) Assessment in behavioural medicine. Brunner-Routledge, Hove, pp 353–370
De Vries J, Michielsen HJ, Van Heck GL (2003) Assessment of fatigue among working people: a comparison of six questionnaires. Occup Environ Med 60(Suppl 1):i10–i15
De Vries J, Michielsen H, Van Heck GL, Drent M (2004) Measuring fatigue in sarcoidosis: the fatigue assessment scale (FAS). Br J Health Psychol 9:279–291
Drost G, Blok JH, Stegeman DF, van Dijk JP, van Engelen BGM, Zwarts MJ (2001) Propagation disturbance of motor unit action potentials during transient paresis in generalized myotonia: a high-density surface EMG study. Brain 124:352–360
Eulenburg A (1886) Uber einer familiare durch 6 Generationen verfolgbare Form kongenitaler Paramyotonie. Neurol Zbl 5:265–272
Forbes A, While A, Mathes L, Griffiths P (2006) Health problems and health-related quality of life in people with multiple sclerosis. Clin Rehabil 20:67–78
Heatwole CR, Moxley RT 3rd (2007) The nondystrophic myotonias. Neurotherapeutics 4:238–251
Herlofson K, Larsen JP (2003) The influence of fatigue on health-related quality of life in patients with Parkinson’s disease. Acta Neurol Scand 107:1–6
Herndon JEI, Harrell FEJ (1990) The restricted cubic spline hazard model. Stat Theory Methods 19:639–663
Kalkman JS, Schillings ML, van der Werf SP et al (2005) Experienced fatigue in facioscapulohumeral dystrophy, myotonic dystrophy and HMSN-I. J Neurol Neurosurg Psychiat 76:1406–1409
Kempen GI, Ormel J, Brilman EI, Relyveld J (1997) Adaptive responses among Dutch elderly: the impact of eight chronic medical conditions on health-related quality of life. Am J Public Health 87:38–44
Lehmann-Horn F, Rüdel R (1997) Non-dystrophic myotonias and periodic paralyses. In: Emery AEH (ed) Diagnostic criteria for neuromuscular disorders. Royal Society of Medicine Press, London, pp 31–36
Lehmann-Horn F, Rüdel R, Jurkat-Rott K (2004) Nondystrophic myotonias and periodic paralyses. In: Engel AG, Franzini-Armstrong C (eds) Myology, 3rd edn. Mc Graw-Hill Company, New York, pp 1257–1300
Lerche H, Heine R, Pika U et al (1993) Human sodium channel myotonia: slowed channel inactivation due to substitutions for glycine within the III-IV linker. J Physiol 470:13–22
Merkies IS, Schmitz PI, Samijn JP, van der Meché FG, van Doorn PA (1999) Fatigue in immune-mediated polyneuropathies. European Inflammatory Neuropathy Cause and Treatment (INCAT) Group. Neurology 53:1648–1654
Michielsen HJ, De Vries J, Van Heck GL, v/d Vijver FJR, Sijtsma K (2004) Examination of the dimensionality of fatigue: the construction of the fatigue assessment scale (FAS). Eur J Psychol Assess 20:39–48
Nunnally JC (1978) Psychometric theory. Mc Graw Hill, New York
Patti F, Cacopardo M, Palermo F et al (2003) Health-related quality of life and depression in an Italian sample of multiple sclerosis patients. J Neurol Sci 211:55–62
Paul RH, Cohen RA, Goldstein JM, Gilchrist JM (2000) Fatigue and its impact on patients with myasthenia gravis. Muscle Nerve 23:1402–1406
Quittenbaum BH, Grahn B (2004) Quality of life and pain in Parkinson’s disease: a controlled cross-sectional study. Parkinsonism Relat Disord 10:129–136
Ricker K, Haass A, Hertel G, Mertens HG (1978) Transient muscular weakness in severe recessive myotonia congenital. Improvement of isometric muscle force by drugs relieving myotonic stiffness. J Neurol 218:253–262
Ricker K, Moxley RT 3rd, Heine R, Lehmann-Horn F (1994) Myotonia fluctuans. A third type of muscle sodium channel disease. Arch Neurol 51:1095–1102
Rosenfeld J, Sloan-Brown K, George AL Jr (1997) A novel muscle sodium channel mutation causes painful congenital myotonia. Ann Neurol 42:811–814
Rüdel R, Lehmann-Horn F (1997) Paramyotonia, potassium-aggravated myotonias, periodic paralyses In: 37th ENMC International Workshop, Naarden, the Netherlands, 8–10 December 1995. Neuromuscul Disord 7:127–132
Ruhland JL, Shields RK (1997) The effects of a home exercise program on impairment and health-related quality of life in persons with chronic peripheral neuropathies. Phys Ther 77:1026–1039
Solari A, Radice D (2001) Health status of people with multiple sclerosis: a community mail survey. Neurol Sci 22:307–315
Sunnerhagen KS, Grimby G (2001) Muscular effects in late polio. Acta Physiol Scand 171:335–340
Trip J, Drost G, Verbove DJ et al (2008) In tandem analysis of CLCN1 and SCN4A greatly enhances mutation detection in families with non-dystrophic myotonia. Eur J Hum Genet 16:921–929
Trip J, Drost G, Ginjaar HB et al Redefining the clinical phenotypes of non-dystrophic myotonic syndromes. Submitted
Trudell RG, Kaiser KK, Griggs RC (1987) Acetazolamide-responsive myotonia congenita. Neurology 37:488–491
Van den Berg JP, Kalmijn S, Lindeman E et al (2005) Multidisciplinary ALS care improves quality of life in patients with ALS. Neurology 65:1264–1267
Wagner S, Deymeer F, Kürz LL et al (1998) The dominant chloride channel mutant G200R causing fluctuating myotonia: clinical findings, electrophysiology, and channel pathology. Muscle Nerve 21:1122–1128
Ware JE Jr, Snow KK, Kosinski M, Gandek B (1993) The SF-36 health survey. Manual and interpretation guide. The Health Institute, New England Medical Center, Boston
Ware JE Jr, Kosinski M, Keller SD (1994) SF-36 physical and mental health summeray scales: a user’s manual. The Health Institute, New England Medical Center, Boston
Ware JE Jr, Gandek B, Kosinski M et al (1998) The equivalence of SF-36 summery health scores estimated using standard and country-specific algorithms in 10 countries: results from the IQOLA Project. International Quality of Life Assessment. J Clin Epidemiol 51:1167–1170
Acknowledgments
We would like to thank Ingemar Merkies for his support to the statistics and the first draft of this manuscript.
Conflict of interest statement
None.
Funding
Prinses Beatrix Fonds (MAR04-0118), The Netherlands.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Trip, J., de Vries, J., Drost, G. et al. Health status in non-dystrophic myotonias: close relation with pain and fatigue. J Neurol 256, 939–947 (2009). https://doi.org/10.1007/s00415-009-5049-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-009-5049-y