Abstract
Mild traumatic brain injury (TBI), which is defined as a head trauma resulting in a brief loss of consciousness and/or alteration of mental state, is usually benign, but occasionally causes persistent and sometimes progressive symptoms. Whether a threshold for the amount of brain injury and/or individual vulnerability might contribute to the development of these long-term consequences is unknown. Furthermore, reliable diagnostic methods that can establish whether a blow to the head has affected the brain (and in what way) are lacking. In this Review, we discuss potential biomarkers of injury to different structures and cell types in the CNS that can be detected in body fluids. We present arguments in support of the need for further development and validation of such biomarkers, and for their use in assessing patients with head trauma in whom the brain might have been affected. Specifically, we focus on the need for such biomarkers in the management of sports-related concussion, the most common cause of mild TBI in young individuals, to prevent long-term neurological sequelae due to concussive or subconcussive blows to the head.
Key Points
-
Biomarkers of neuronal, axonal and astroglial damage could be used to diagnose mild traumatic brain injury (TBI) and predict clinical outcomes of patients with head trauma
-
Such biomarkers could provide important information for medical counselling of at-risk individuals, such as military personnel and concussed athletes
-
Cerebrospinal fluid markers are preferred over peripheral blood markers, owing to their increased proximity to the brain and decreased susceptibility to the confounding effects of various extracerebral factors
-
Ultrasensitive assays are needed for reliable quantification of CNS-specific biomarkers in blood, as their concentrations are below the lower limit of detection by most standard immunoassays
-
Clinical studies of serial biomarker measurements in conjunction with advanced brain imaging during the acute and subacute phases of mild TBI are warranted
-
Longitudinal studies of biomarkers in patients with chronic or progressive symptoms after TBI might help to clarify the pathogenesis and clinical course of chronic traumatic encephalopathy
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Roozenbeek, B., Maas, A. I. & Menon, D. K. Opinion: Changing patterns in the epidemiology of traumatic brain injury. Nat. Rev. Neurol. http://dx.doi/org/nrneurol.2013.22
American Congress of Rehabilitation Medicine. Definition of mild traumatic brain injury. J. Head Trauma Rehabil. 8, 86–87 (1993).
Blumbergs, P. C. et al. Staining of amyloid precursor protein to study axonal damage in mild head injury. Lancet 344, 1055–1056 (1994).
Browne, K. D., Chen, X. H., Meaney, D. F. & Smith, D. H. Mild traumatic brain injury and diffuse axonal injury in swine. J. Neurotrauma 28, 1747–1755 (2011).
Baugh, C. M. et al. Chronic traumatic encephalopathy: neurodegeneration following repetitive concussive and subconcussive brain trauma. Brain Imaging Behav. 6, 244–254 (2012).
Gavett, B. E., Stern, R. A. & McKee, A. C. Chronic traumatic encephalopathy: a potential late effect of sport-related concussive and subconcussive head trauma. Clin. Sports Med. 30, 179–188 (2011).
Goldstein, L. E. et al. Chronic traumatic encephalopathy in blast-exposed military veterans and a blast neurotrauma mouse model. Sci. Transl. Med. 4, 134ra160 (2012).
McCrory, P. et al. Consensus statement on concussion in sport—the 3rd International Conference on Concussion in Sport held in Zurich, November 2008. Phys. Sportsmed. 37, 141–159 (2009).
Røe, C., Sveen, U., Alvsåker, K. & Bautz-Holter, E. Post-concussion symptoms after mild traumatic brain injury: influence of demographic factors and injury severity in a 1-year cohort study. Disabil. Rehabil. 31, 1235–1243 (2009).
Williams, W. H., Potter, S. & Ryland, H. Mild traumatic brain injury and postconcussion syndrome: a neuropsychological perspective. J. Neurol. Neurosurg. Psychiatry 81, 1116–1122 (2010).
Meaney, D. F. & Smith, D. H. Biomechanics of concussion. Clin. Sports Med. 30, 19–31 (2011).
Smith, D. H. & Meaney, D. F. Axonal damage in traumatic brain injury. The Neuroscientist 6, 483–495 (2000).
Johnson, V. E., Stewart, W. & Smith, D. H. Axonal pathology in traumatic brain injury. Exp. Neurol. (2012).
Wolf, J. A., Stys, P. K., Lusardi, T., Meaney, D. & Smith, D. H. Traumatic axonal injury induces calcium influx modulated by tetrodotoxin-sensitive sodium channels. J. Neurosci. 21, 1923–1930 (2001).
Saatman, K. E., Creed, J. & Raghupathi, R. Calpain as a therapeutic target in traumatic brain injury. Neurotherapeutics 7, 31–42 (2010).
Giza, C. C. & Hovda, D. A. The neurometabolic cascade of concussion. J. Athl. Train. 36, 228–235 (2001).
Barkhoudarian, G., Hovda, D. A. & Giza, C. C. The molecular pathophysiology of concussive brain injury. Clin. Sports Med. 30, 33–48 (2011).
Tang-Schomer, M. D., Patel, A. R., Baas, P. W. & Smith, D. H. Mechanical breaking of microtubules in axons during dynamic stretch injury underlies delayed elasticity, microtubule disassembly, and axon degeneration. FASEB J. 24, 1401–1410 (2010).
Tang-Schomer, M. D., Johnson, V. E., Baas, P. W., Stewart, W. & Smith, D. H. Partial interruption of axonal transport due to microtubule breakage accounts for the formation of periodic varicosities after traumatic axonal injury. Exp. Neurol. 233, 364–372 (2012).
Povlishock, J. T., Becker, D. P., Cheng, C. L. & Vaughan, G. W. Axonal change in minor head injury. J. Neuropathol. Exp. Neurol. 42, 225–242 (1983).
Povlishock, J. T. & Becker, D. P. Fate of reactive axonal swellings induced by head injury. Lab. Invest. 52, 540–552 (1985).
Chen, X. H. et al. Long-term accumulation of amyloid-β, β-secretase, presenilin-1, and caspase-3 in damaged axons following brain trauma. Am. J. Pathol. 165, 357–371 (2004).
Lipton, M. L. et al. Multifocal white matter ultrastructural abnormalities in mild traumatic brain injury with cognitive disability: a voxel-wise analysis of diffusion tensor imaging. J. Neurotrauma 25, 1335–1342 (2008).
Niogi, S. N. et al. Extent of microstructural white matter injury in postconcussive syndrome correlates with impaired cognitive reaction time: a 3T diffusion tensor imaging study of mild traumatic brain injury. AJNR Am. J. Neuroradiol. 29, 967–973 (2008).
Wilde, E. A. et al. Diffusion tensor imaging of acute mild traumatic brain injury in adolescents. Neurology 70, 948–955 (2008).
New Zealand Guidelines Group Staff, Accident Compensation Corporation (N. Z.) Staff. Traumatic Brain Injury: Diagnosis, Acute Management and Rehabilitation (Accident Compensation Corporation, New Zealand, 2006).
Iverson, G. L., Gaetz, M., Lovell, M. R. & Collins, M. W. Cumulative effects of concussion in amateur athletes. Brain Inj. 18, 433–443 (2004).
Brooks, W. M. et al. Metabolic and cognitive response to human traumatic brain injury: a quantitative proton magnetic resonance study. J. Neurotrauma 17, 629–640 (2000).
Anderson, V., Catroppa, C., Morse, S., Haritou, F. & Rosenfeld, J. Recovery of intellectual ability following traumatic brain injury in childhood: impact of injury severity and age at injury. Pediatr. Neurosurg. 32, 282–290 (2000).
Prins, M. L. & Hovda, D. A. Developing experimental models to address traumatic brain injury in children. J. Neurotrauma 20, 123–137 (2003).
Duhaime, A. C. Large animal models of traumatic injury to the immature brain. Dev. Neurosci. 28, 380–387 (2006).
Pinto, P. S., Meoded, A., Poretti, A., Tekes, A. & Huisman, T. A. The unique features of traumatic brain injury in children. Review of the characteristics of the pediatric skull and brain, mechanisms of trauma, patterns of injury, complications, and their imaging findings—part 2. J. Neuroimaging 22, e18–e41 (2012).
Pinto, P. S., Poretti, A., Meoded, A., Tekes, A. & Huisman, T. A. The unique features of traumatic brain injury in children. Review of the characteristics of the pediatric skull and brain, mechanisms of trauma, patterns of injury, complications and their imaging findings—part 1. J. Neuroimaging 22, e1–e17 (2012).
Martland, H. Punch drunk. JAMA 91, 1103–1107 (1928).
Roberts, A. H. Brain Damage in Boxers: a Study of the Prevalence of Traumatic Encephalopathy Among Ex-Professional Boxers (Pitman Medical Scientific Publications, London, 1969).
Jordan, B. D. et al. Apolipoprotein E ε4 associated with chronic traumatic brain injury in boxing. JAMA 278, 136–140 (1997).
Stern, R. A. et al. Long-term consequences of repetitive brain trauma: chronic traumatic encephalopathy. PM R 3, S460–S467 (2011).
Smith, D. H., Johnson, V. E. & Stewart, W. The chronic neuropathologies of single and repetitive traumatic brain injury: potential substrates of dementia? Nat. Rev. Neurol. (in press).
Gavett, B. E. et al. Clinical appraisal of chronic traumatic encephalopathy: current perspectives and future directions. Curr. Opin. Neurol. 24, 525–531 (2011).
Jordan, B. D. Chronic traumatic brain injury associated with boxing. Semin. Neurol. 20, 179–185 (2000).
Mendez, M. F. The neuropsychiatric aspects of boxing. Int. J. Psychiatry Med. 25, 249–262 (1995).
Roberts, G. W., Allsop, D. & Bruton, C. The occult aftermath of boxing. J. Neurol. Neurosurg. Psychiatry 53, 373–378 (1990).
Tokuda, T., Ikeda, S., Yanagisawa, N., Ihara, Y. & Glenner, G. G. Re-examination of ex-boxers' brains using immunohistochemistry with antibodies to amyloid β-protein and tau protein. Acta Neuropathol. 82, 280–285 (1991).
Johnson, V. E., Stewart, W. & Smith, D. H. Traumatic brain injury and amyloid-β pathology: a link to Alzheimer's disease? Nat. Rev. Neurosci. 11, 361–370 (2010).
Johnson, V. E., Stewart, W. & Smith, D. H. Widespread tau and amyloid-β pathology many years after a single traumatic brain injury in humans. Brain Pathol. 22, 142–149 (2012).
Johnson, V. E., Stewart, W., Trojanowski, J. Q. & Smith, D. H. Acute and chronically increased immunoreactivity to phosphorylation-independent but not pathological TDP-43 after a single traumatic brain injury in humans. Acta Neuropathol. 122, 715–726 (2011).
Jordan, B. D. Clinical spectrum of sports-related traumatic brain injury. Nat. Rev. Neurol. (in press).
Blennow, K., Hampel, H., Weiner, M. & Zetterberg, H. Cerebrospinal fluid and plasma biomarkers in Alzheimer disease. Nat. Rev. Neurol. 6, 131–144 (2010).
Abbott, N. J., Rönnbäck, L. & Hansson, E. Astrocyte-endothelial interactions at the blood–brain barrier. Nat. Rev. Neurosci. 7, 41–53 (2006).
Tibbling, G., Link, H. & Ohman, S. Principles of albumin and IgG analyses in neurological disorders. I. Establishment of reference values. Scand. J. Clin. Lab. Invest. 37, 385–390 (1977).
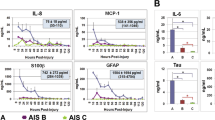
Csuka, E. et al. IL-10 levels in cerebrospinal fluid and serum of patients with severe traumatic brain injury: relationship to IL-6, TNF-α, TGF-β1 and blood–brain barrier function. J. Neuroimmunol. 101, 211–221 (1999).
Kossmann, T. et al. Intrathecal and serum interleukin-6 and the acute-phase response in patients with severe traumatic brain injuries. Shock 4, 311–317 (1995).
Blennow, K. et al. No neurochemical evidence of brain injury after blast overpressure by repeated explosions or firing heavy weapons. Acta Neurol. Scand. 123, 245–251 (2011).
Zetterberg, H. et al. Neurochemical aftermath of amateur boxing. Arch. Neurol. 63, 1277–1280 (2006).
Semple, B. D., Bye, N., Rancan, M., Ziebell, J. M. & Morganti-Kossmann, M. C. Role of CCL2 (MCP-1) in traumatic brain injury (TBI): evidence from severe TBI patients and CCL2−/− mice. J. Cereb Blood Flow Metab. 30, 769–782 (2010).
Kirchhoff, C. et al. Cerebrospinal IL-10 concentration is elevated in non-survivors as compared to survivors after severe traumatic brain injury. Eur. J. Med. Res. 13, 464–468 (2008).
Goodman, J. C., Van, M., Gopinath, S. P. & Robertson, C. S. Pro-inflammatory and pro-apoptotic elements of the neuroinflammatory response are activated in traumatic brain injury. Acta Neurochir. Suppl. 102, 437–439 (2008).
Buttram, S. D. et al. Multiplex assessment of cytokine and chemokine levels in cerebrospinal fluid following severe pediatric traumatic brain injury: effects of moderate hypothermia. J. Neurotrauma 24, 1707–1717 (2007).
Phillips, D. J. et al. Activin A release into cerebrospinal fluid in a subset of patients with severe traumatic brain injury. J. Neurotrauma 23, 1283–1294 (2006).
Maier, B. et al. Delayed elevation of soluble tumor necrosis factor receptors p75 and p55 in cerebrospinal fluid and plasma after traumatic brain injury. Shock 26, 122–127 (2006).
Shiozaki, T. et al. Cerebrospinal fluid concentrations of anti-inflammatory mediators in early-phase severe traumatic brain injury. Shock 23, 406–410 (2005).
Singhal, A. et al. Association between cerebrospinal fluid interleukin-6 concentrations and outcome after severe human traumatic brain injury. J. Neurotrauma 19, 929–937 (2002).
Stahel, P. F. et al. Intrathecal levels of complement-derived soluble membrane attack complex (sC5b-9) correlate with blood–brain barrier dysfunction in patients with traumatic brain injury. J. Neurotrauma 18, 773–781 (2001).
Bell, M. J. et al. Interleukin-6 and interleukin-10 in cerebrospinal fluid after severe traumatic brain injury in children. J. Neurotrauma 14, 451–457 (1997).
Trojanowski, J. Q., Schuck, T., Schmidt, M. L. & Lee, V. M. Distribution of tau proteins in the normal human central and peripheral nervous system. J. Histochem. Cytochem. 37, 209–215 (1989).
Friede, R. L. & Samorajski, T. Axon caliber related to neurofilaments and microtubules in sciatic nerve fibers of rats and mice. Anat. Rec. 167, 379–387 (1970).
Franz, G. et al. Amyloid β1–42 and tau in cerebrospinal fluid after severe traumatic brain injury. Neurology 60, 1457–1461 (2003).
Zemlan, F. P. et al. C-tau biomarker of neuronal damage in severe brain injured patients: association with elevated intracranial pressure and clinical outcome. Brain Res. 947, 131–139 (2002).
Blennow, K. & Nellgård, B. Amyloid β1–42 and tau in cerebrospinal fluid after severe traumatic brain injury. Neurology 62, 159–160 (2004).
Ost, M. et al. Initial CSF total tau correlates with 1-year outcome in patients with traumatic brain injury. Neurology 67, 1600–1604 (2006).
Neselius, S. et al. CSF-biomarkers in Olympic boxing: diagnosis and effects of repetitive head trauma. PLoS ONE 7, e33606 (2012).
Liu, Q. et al. Neurofilament proteins in neurodegenerative diseases. Cell. Mol. Life Sci. 61, 3057–3075 (2004).
Siman, R. et al. A panel of neuron-enriched proteins as markers for traumatic brain injury in humans. J. Neurotrauma 26, 1867–1877 (2009).
Olsson, B., Zetterberg, H., Hampel, H. & Blennow, K. Biomarker-based dissection of neurodegenerative diseases. Prog. Neurobiol. 4, 520–534 (2011).
Scarna, H. et al. Neuron-specific enolase as a marker of neuronal lesions during various comas in man. Neurochem. Int. 4, 405–411 (1982).
Bohmer, A. E. et al. Neuron-specific enolase, S100B, and glial fibrillary acidic protein levels as outcome predictors in patients with severe traumatic brain injury. Neurosurgery 68, 1624–1631 (2011).
Chiaretti, A. et al. NGF, DCX, and NSE upregulation correlates with severity and outcome of head trauma in children. Neurology 72, 609–616 (2009).
Varma, S. et al. F2-isoprostane and neuron-specific enolase in cerebrospinal fluid after severe traumatic brain injury in infants and children. J. Neurotrauma 20, 781–786 (2003).
Berger, R. P. et al. Neuron-specific enolase and S100B in cerebrospinal fluid after severe traumatic brain injury in infants and children. Pediatrics 109, E31 (2002).
Ross, S. A., Cunningham, R. T., Johnston, C. F. & Rowlands, B. J. Neuron-specific enolase as an aid to outcome prediction in head injury. Br. J. Neurosurg. 10, 471–476 (1996).
Berger, R. P. et al. Identification of inflicted traumatic brain injury in well-appearing infants using serum and cerebrospinal markers: a possible screening tool. Pediatrics 117, 325–332 (2006).
Ramont, L. et al. Effects of hemolysis and storage condition on neuron-specific enolase (NSE) in cerebrospinal fluid and serum: implications in clinical practice. Clin. Chem. Lab. Med. 43, 1215–1217 (2005).
Moore, B. W. & McGregor, D. Chromatographic and electrophoretic fractionation of soluble proteins of brain and liver. J. Biol. Chem. 240, 1647–1653 (1965).
Isobe, T., Ishioka, N. & Okuyama, T. Structural relation of two S-100 proteins in bovine brain; subunit composition of S.-100A protein. Eur. J. Biochem. 115, 469–474 (1981).
Nylen, K. et al. Serum levels of S100B, S100A1B and S100BB are all related to outcome after severe traumatic brain injury. Acta Neurochir. (Wien) 150, 221–227 (2008).
Czeiter, E. et al. Brain injury biomarkers may improve the predictive power of the IMPACT outcome calculator. J. Neurotrauma 29, 1770–1778 (2012).
McKenzie, J. E., Gentleman, S. M., Roberts, G. W., Graham, D. I. & Royston, M. C. Increased numbers of β APP-immunoreactive neurones in the entorhinal cortex after head injury. Neuroreport 6, 161–164 (1994).
Sherriff, F. E., Bridges, L. R. & Sivaloganathan, S. Early detection of axonal injury after human head trauma using immunocytochemistry for β-amyloid precursor protein. Acta Neuropathol. 87, 55–62 (1994).
Gentleman, S. M. et al. Axonal injury: a universal consequence of fatal closed head injury? Acta Neuropathol. 89, 537–543 (1995).
Ahlgren, S., Li, G. L. & Olsson, Y. Accumulation of β-amyloid precursor protein and ubiquitin in axons after spinal cord trauma in humans: immunohistochemical observations on autopsy material. Acta Neuropathol. 92, 49–55 (1996).
Gleckman, A. M., Bell, M. D., Evans, R. J. & Smith, T. W. Diffuse axonal injury in infants with nonaccidental craniocerebral trauma: enhanced detection by β-amyloid precursor protein immunohistochemical staining. Arch. Pathol. Lab. Med. 123, 146–151 (1999).
McKenzie, K. J. et al. Is β-APP a marker of axonal damage in short-surviving head injury? Acta Neuropathol. 92, 608–613 (1996).
Smith, D. H., Chen, X. H., Iwata, A. & Graham, D. I. Amyloid β accumulation in axons after traumatic brain injury in humans. J. Neurosurg. 98, 1072–1077 (2003).
Uryu, K. et al. Multiple proteins implicated in neurodegenerative diseases accumulate in axons after brain trauma in humans. Exp. Neurol. 208, 185–192 (2007).
Chen, X. H., Johnson, V. E., Uryu, K., Trojanowski, J. Q. & Smith, D. H. A lack of amyloid β plaques despite persistent accumulation of amyloid β in axons of long-term survivors of traumatic brain injury. Brain Pathol. 19, 214–223 (2009).
Roberts, G. W., Gentleman, S. M., Lynch, A. & Graham, D. I. β A4 amyloid protein deposition in brain after head trauma. Lancet 338, 1422–1423 (1991).
Graham, D. I., Gentleman, S. M., Lynch, A. & Roberts, G. W. Distribution of β-amyloid protein in the brain following severe head injury. Neuropathol. Appl. Neurobiol. 21, 27–34 (1995).
Horsburgh, K. et al. β-amyloid (Aβ)42(43), Aβ42, Aβ40 and apoE immunostaining of plaques in fatal head injury. Neuropathol. Appl. Neurobiol. 26, 124–132 (2000).
Raby, C. A. et al. Traumatic brain injury increases β-amyloid peptide1–42 in cerebrospinal fluid. J. Neurochem. 71, 2505–2509 (1998).
Olsson, A. et al. Marked increase of β-amyloid1–42 and amyloid precursor protein in ventricular cerebrospinal fluid after severe traumatic brain injury. J. Neurol. 251, 870–876 (2004).
Mortberg, E. et al. Plasma tau protein in comatose patients after cardiac arrest treated with therapeutic hypothermia. Acta Anaesthesiol. Scand. 55, 1132–1138 (2011).
Randall, J. et al. Tau proteins in serum predict neurological outcome after hypoxic brain injury from cardiac arrest: results of a pilot study. Resuscitation http://dx.doi.org/10.1016/j.resuscitation.2012.07.027.
Rissin, D. M. et al. Single-molecule enzyme-linked immunosorbent assay detects serum proteins at subfemtomolar concentrations. Nat. Biotechnol. 28, 595–599 (2010).
Mondello, S. et al. Blood-based diagnostics of traumatic brain injuries. Expert Rev. Mol. Diagn. 11, 65–78 (2011).
Kovesdi, E. et al. Update on protein biomarkers in traumatic brain injury with emphasis on clinical use in adults and pediatrics. Acta Neurochir. (Wien) 152, 1–17 (2010).
Mussack, T. et al. Significance of Elecsys S100 immunoassay for real-time assessment of traumatic brain damage in multiple trauma patients. Clin. Chem. Lab. Med. 44, 1140–1145 (2006).
Rothoerl, R. D. & Woertgen, C. High serum S100B levels for trauma patients without head injuries. Neurosurgery 49, 1490–1493 (2001).
Anderson, R. E., Hansson, L. O., Nilsson, O., Dijlai-Merzoug, R. & Settergren, G. High serum S100B levels for trauma patients without head injuries. Neurosurgery 48, 1255–1260 (2001).
Romner, B. & Ingebrigtsen, T. High serum S100B levels for trauma patients without head injuries. Neurosurgery 49, 1490–1493 (2001).
Stalnacke, B. M., Ohlsson, A., Tegner, Y. & Sojka, P. Serum concentrations of two biochemical markers of brain tissue damage S-100B and neurone specific enolase are increased in elite female soccer players after a competitive game. Br. J. Sports Med. 40, 313–316 (2006).
Blyth, B. J. et al. Elevated serum ubiquitin carboxy-terminal hydrolase L1 is associated with abnormal blood–brain barrier function after traumatic brain injury. J. Neurotrauma 28, 2453–2462 (2011).
Metting, Z., Wilczak, N., Rodiger, L. A., Schaaf, J. M. & van der Naalt, J. GFAP and S100B in the acute phase of mild traumatic brain injury. Neurology 78, 1428–1433 (2012).
Berger, R. P. et al. Serum neuron-specific enolase, S100B, and myelin basic protein concentrations after inflicted and noninflicted traumatic brain injury in children. J. Neurosurg. 103, 161–68 (2005).
Zurek, J. & Fedora, M. The usefulness of S100B, NSE, GFAP, NF-H, secretagogin and Hsp70 as a predictive biomarker of outcome in children with traumatic brain injury. Acta Neurochir. (Wien) 154, 193–103 (2012).
Zurek, J., Bartlova, L. & Fedora, M. Hyperphosphorylated neurofilament NF-H as a predictor of mortality after brain injury in children. Brain Inj. 25, 221–226 (2011).
Tisdall, M. & Petzold, A. Comment on “chronic traumatic encephalopathy in blast-exposed military veterans and a blast neurotrauma mouse model”. Sci. Transl. Med. 4, 157le158 (2012).
Riederer, B. M., Zagon, I. S. & Goodman, S. R. Brain spectrin(240/235) and brain spectrin(240/235E): two distinct spectrin subtypes with different locations within mammalian neural cells. J. Cell Biol. 102, 2088–2097 (1986).
Pike, B. R. et al. Accumulation of non-erythroid α II-spectrin and calpain-cleaved α II-spectrin breakdown products in cerebrospinal fluid after traumatic brain injury in rats. J. Neurochem. 78, 1297–1306 (2001).
Pineda, J. A. et al. Clinical significance of αII-spectrin breakdown products in cerebrospinal fluid after severe traumatic brain injury. J. Neurotrauma 24, 354–366 (2007).
Farkas, O. et al. Spectrin breakdown products in the cerebrospinal fluid in severe head injury—preliminary observations. Acta Neurochir. (Wien) 147, 855–861 (2005).
Mondello, S. et al. αII-spectrin breakdown products (SBDPs): diagnosis and outcome in severe traumatic brain injury patients. J. Neurotrauma 27, 1203–1213 (2010).
Wilkinson, K. D. et al. The neuron-specific protein PGP 9.5 is a ubiquitin carboxyl-terminal hydrolase. Science 246, 670–673 (1989).
Papa, L. et al. Serum levels of ubiquitin C-terminal hydrolase distinguish mild traumatic brain injury from trauma controls and are elevated in mild and moderate traumatic brain injury patients with intracranial lesions and neurosurgical intervention. J. Trauma Acute Care Surg. 72, 1335–1344 (2012).
Ottens, A. K. et al. Neuroproteomics in neurotrauma. Mass Spectrom. Rev. 25, 380–408 (2006).
Pasinetti, G. M., Ho, L., Dooley, C., Abbi, B. & Lange, G. Select non-coding RNA in blood components provide novel clinically accessible biological surrogates for improved identification of traumatic brain injury in OEF/OIF veterans. Am. J. Neurodegener. Dis. 1, 88–98 (2012).
Corsellis, J. A., Bruton, C. J. & Freeman-Browne, D. The aftermath of boxing. Psychol. Med. 3, 270–303 (1973).
Pollock, N. J., Mirra, S. S., Binder, L. I., Hansen, L. A. & Wood, J. G. Filamentous aggregates in Pick's disease, progressive supranuclear palsy, and Alzheimer's disease share antigenic determinants with microtubule-associated protein, tau. Lancet 2, 1211 (1986).
Hampel, H. et al. Measurement of phosphorylated tau epitopes in the differential diagnosis of Alzheimer disease: a comparative cerebrospinal fluid study. Arch. Gen. Psychiatry 61, 95–102 (2004).
Hall, S. et al. Accuracy of a panel of 5 cerebrospinal fluid biomarkers in the differential diagnosis of patients with dementia and/or parkinsonian disorders. Arch. Neurol., 27, 1–8 (2012).
Dickson, D. W., Kouri, N., Murray, M. E. & Josephs, K. A. Neuropathology of frontotemporal lobar degeneration-tau (FTLD-tau). J. Mol. Neurosci. 45, 384–389 (2011).
King, A. et al. Abnormal TDP-43 expression is identified in the neocortex in cases of dementia pugilistica, but is mainly confined to the limbic system when identified in high and moderate stages of Alzheimer's disease. Neuropathology 30, 408–419 (2010).
McKee, A. C. et al. TDP-43 proteinopathy and motor neuron disease in chronic traumatic encephalopathy. J. Neuropathol. Exp. Neurol. 69, 918–929 (2010).
Neumann, M. et al. Ubiquitinated TDP-43 in frontotemporal lobar degeneration and amyotrophic lateral sclerosis. Science 314, 130–133 (2006).
Geser, F. et al. On the development of markers for pathological TDP-43 in amyotrophic lateral sclerosis with and without dementia. Prog. Neurobiol. 95, 649–662 (2011).
Guerrero, A. F. & Alfonso, A. Traumatic brain injury-related hypopituitarism: a review and recommendations for screening combat veterans. Mil. Med. 175, 574–580 (2010).
Kelestimur, F. et al. Boxing as a sport activity associated with isolated GH deficiency. J. Endocrinol. Invest. 27, RC28–RC32 (2004).
Tanriverdi, F. et al. Brief communication: pituitary volume and function in competing and retired male boxers. Ann. Intern. Med. 148, 827–831 (2008).
Tanriverdi, F. et al. Kickboxing sport as a new cause of traumatic brain injury-mediated hypopituitarism. Clin. Endocrinol. (Oxf.) 66, 360–366 (2007).
Wilkinson, C. W. et al. High prevalence of chronic pituitary and target-organ hormone abnormalities after blast-related mild traumatic brain injury. Front. Neurol. 3, 11 (2012).
Acknowledgements
The authors' research work is supported by the Swedish Research Council and Swedish State Support for Clinical Research (H. Zetterberg, K. Blennow), the Wolfson Foundation (H. Zetterberg) and NIH grants R01 NS038104, P01 NS056202 and R03 AG038911 (D. H. Smith).
Author information
Authors and Affiliations
Contributions
H. Zetterberg wrote the article. H. Zetterberg, D. H. Smith and K. Blennow contributed equally to researching data for the article, discussion of the content, and review and editing of the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Zetterberg, H., Smith, D. & Blennow, K. Biomarkers of mild traumatic brain injury in cerebrospinal fluid and blood. Nat Rev Neurol 9, 201–210 (2013). https://doi.org/10.1038/nrneurol.2013.9
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrneurol.2013.9
This article is cited by
-
Plasma neurofilament light admission levels and development of axonal pathology in mild traumatic brain injury
BMC Neurology (2023)
-
Plasma phospho-tau in Alzheimer’s disease: towards diagnostic and therapeutic trial applications
Molecular Neurodegeneration (2023)
-
The longitudinal biochemical profiling of TBI in a drop weight model of TBI
Scientific Reports (2023)
-
Neurobiochemical, Peptidomic, and Bioinformatic Approaches to Characterize Tauopathy Peptidome Biomarker Candidates in Experimental Mouse Model of Traumatic Brain Injury
Molecular Neurobiology (2023)
-
Diffusion Imaging of Sport-related Repetitive Head Impacts—A Systematic Review
Neuropsychology Review (2023)